Early pregnancy health and care

Good health and care in pregnancy is very important for both you and your baby, and early pregnancy is particularly important. This information brochure outlines the key issues in early pregnancy health and care, as well as information about what to do next.
WHEN SHOULD I SEE A DOCTOR?
Ideally you should see a doctor before you become pregnant in order to discuss any tests necessary (for example whether you are immune to Rubella or Chickenpox), as well as to discuss any medical problems, medications, and to get advice on supplements in pregnancy.
If this hasn’t happened because your pregnancy was unplanned or unexpected, then when you first find out you are pregnant is a good time to visit your GP. They can give you further information, answer questions, discuss the important routine blood tests done in early pregnancy, and refer you to whoever will be undertaking your pregnancy care as needed.
HOW IS THE LENGTH OF A PREGNANCY CALCULATED?
Pregnancy is counted from the first day of your last normal menstrual period and lasts about 40 weeks from that time.
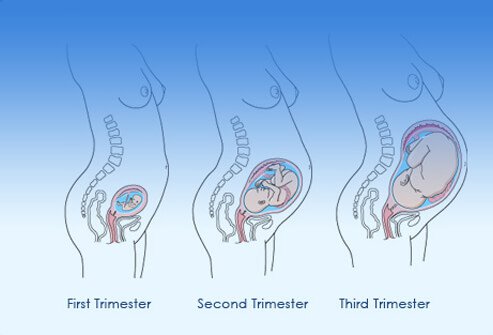
PREGNANCY is divided into 3 trimesters:
- First trimester: up to 12 weeks
- Second trimester: 12 to 24 weeks
- Third trimester: 24 to 40 weeks
HEALTH IN EARLY PREGNANCY NUTRITION IN PREGNANCY
Pregnancy places significant demands on your body and good nutrition during this time is very important for your health and the health of your developing baby.
Only a very small increase in the amount of food or calories is required, it is the quality of the diet which really matters. The need for protein, iron, iodine, and folate do increase in pregnancy however, overall a healthy balanced diet including food from all food groups is what is needed.
A vegetarian diet can meet the needs of your pregnancy as long as you take care to include enough protein, iron, vitamin B12, and calcium-containing foods. For further information on diet in pregnancy talk to your GP or a dietician.
FOLATE
Folate (also known as folic acid) is one of the B-group vitamins and is essential for the healthy development of a foetus in early pregnancy. Folate can reduce the incidence of serious defects known as neural tube defects (such as spina bifida). While folate is found naturally in foods such as leafy green vegetables, broccoli, brussel sprouts, oranges, bananas, strawberries, and legumes, most women do not eat enough in their diet so a supplement is very important and always recommended. Taking 0.5mg (500mcg) of folate daily for 12 weeks before conception and during the first 12 weeks of pregnancy is advised. It is available in tablet form from any pharmacy. In some women, for example women with diabetes or epilepsy, a higher dose of folic acid may be recommended.
IODINE
Iodine is an essential nutrient for humans. It is especially important for the development of a baby’s brain and the nervous system during pregnancy and in infancy. It is recommended that all pregnant and breastfeeding women take an iodine supplement of 150 micrograms a day. Discuss this with your GP to make sure that you have no contraindications.
IRON
Iron is an essential nutrient needed by the body to make red blood cells which carry oxygen around the body. Iron requirements increase during pregnancy and a deficiency can lead to tiredness, dizziness, and decreased resistance to infection. Pregnant women can usually get enough iron from food, and eating iron rich foods is recommended rather than taking a supplement. However some women may find that they need iron supplementation, such as those who have a vegetarian or vegan diet, have a history of iron deficiency, or have a multiple pregnancy. Taking iron supplements a couple of times a week is recommended rather than a daily dose. Iron supplements can cause side effects so if you think you may need one discuss it with your GP.

The most important source of vitamin D is sunlight.
VITAMIN D
Vitamin D is a nutrient that helps to maintain the strength of bone and muscle, and to assist you with absorbing calcium. It also helps babies to develop strong bones during pregnancy. The most important source of vitamin D is sunlight. In summer, normal daily exposure to sunlight should supply adequate vitamin D without putting you at increased risk of skin cancer. In winter the recommended exposure is 2-3 hours a week. Darker skinned people require longer exposure to sunlight to get enough vitamin D.
VITAMIN B12
Vitamin B12 is one of the B group vitamins and is found in meat and eggs. It is essential for the development of the brain and nervous system of babies. Some women are at an increased risk of B12 deficiency, including women with a family history of B12 deficiency, with conditions affection absorption, or who are strict vegetarians or vegan. These women should consider supplementation with Vitamin B12 in pregnancy and during breastfeeding. B12 is available in tablet form from any pharmacy. If you are at risk of B12 deficiency discuss this with your GP.
CALCIUM
Calcium is an essential mineral and is important during pregnancy and breastfeeding because it is needed for the formation of the baby’s bones. Calcium supplements are not considered necessary in pregnancy; just make sure that you are getting enough calcium as part of a healthy diet. Dairy foods, such as milk, cheese and yoghurt, and calcium-fortified soymilk are excellent dietary sources of calcium. 3 serves a day are recommended.
MULTIVITAMIN SUPPLEMENTS
There is no evidence that taking a multivitamin in pregnancy is useful, and there is some evidence that taken in the last trimester there may be some harm associated with it. A healthy balanced diet should be adequate for most women. If you do still wish to take a multivitamin discuss this with your GP, midwife, or obstetrician first.
MERCURY IN FISH
Fish can be a valuable source of protein in pregnancy, however, some fish contain mercury which can cause developmental delays in children who have been exposed during pregnancy. Pregnant women need to limit the amount of fish they eat which contain high levels of mercury. These fish include: flake, ray, swordfish, barramundi, gemfish, orange roughy, ling and southern bluefin tuna.

WATER
Pregnant women have an increased need for water because of changing needs in the body as well as the needs of the baby so it is important to make sure that you are drinking plenty of water.

You can still enjoy your coffee in moderation.
CAFFEINE
Low to moderate consumption of caffeine in pregnancy is considered safe.
WEIGHT GAIN IN PREGNANCY
Weight gain in pregnancy is very normal, it is due to changes in body tissue, larger breasts and uterus, increases in fluid and blood volume, and the weight of the developing foetus. However, the amount of weight gain recommended will depend on your pre-pregnancy weight. Weight gain varies between women. Average weight gain is usually between 11.5 and 16 kilos. Most women gain around 1 to 2 kilos in the first 3 months, and 1 to 2 kilos a month for the last 6 months.
It is important to not try to lose weight in pregnancy as this can affect the health of the baby, however gaining too much weight can also cause health problems for you. If you are concerned about weight discuss this with your GP or with a dietician.
For women who are underweight, additional serves of the five food groups may contribute to healthy weight gain. For women who are overweight or obese, limiting additional serves and avoiding energy-dense foods may limit excessive weight gain. Weight-loss diets are not recommended during pregnancy.
FOOD SAFETY IN PREGNANCY
A woman’s immune system is lower in pregnancy and there is a slightly increased risk of pregnant women developing a foodborne illness. These illnesses include listeria, salmonella, campylobacter, and toxoplasmosis. These illnesses can be dangerous for the baby. It is therefore important to take steps to reduce the risk of becoming infected.
AVOIDING FOODBORNE ILLNESSES DURING PREGNANCY
Eat mainly freshly prepared and cooked foods and:
- Avoid chilled seafood such as smoked salmon, mussels, oysters, prawns or raw seafood such as sushi.
- Avoid pre-prepared or pre-packaged food from buffets, salad bars and sandwich bars.
- Be cautious with deli meats such as pate, ham, salami, or pre-cooked and diced chicken.
- Avoid undercooked meat or poultry.
- Avoid unpasteurised milk or foods made from unpasteurised milk.
- Avoid soft-serve ice-creams.
- Avoid soft cheeses, such as brie, camembert, ricotta and feta (these are safe if cooked and served hot). Hard cheeses such as cheddar are fine.
- Avoid ready-to-eat foods, including leftover meats, which have been refrigerated for more than one day.
- Avoid dips and salad dressings in which vegetables may have been dipped.
- Avoid pre-cut and pre-packaged vegetables or fruit.
- Do not eat raw sprouts.
- Only eat cooked eggs and avoid products made with raw eggs, such as mayonnaise or aioli.
PRACTICE GOOD FOOD/HAND HYGIENE
Follow good food handling practices such as regular handwashing, washing fruit and vegetables before eating or cooking, keeping surfaces, cutting boards and implements clean, and keeping raw meat separate from other foods.
TOXOPLASMOSIS
This is a parasite normally found in birds and mammals (mainly cats). It is also found in raw pork and lamb. Infection during pregnancy can cause birth defects in the foetus. To reduce risk of exposure to toxoplasmosis avoid close contact with cats, do not change litter trays, wear gloves during gardening, and avoid uncovered sandpits where cat faeces may be found.
EXERCISE IN EARLY PREGNANCY
Low to moderate-intensity exercise in pregnancy can be very beneficial, and has been shown to have a range of health benefits.
However, it is advisable to avoid any physical activity that may risk falls, abdominal trauma, or excessive strain on your joints such as high impact sports and contact sports. Scuba diving is also not advised. If you have any physical problems or conditions which may interfere with you exercising always discuss it with your GP or midwife first.
MEDICATIONS/DRUGS
While some medications are quite safe to use in pregnancy, there are medications and prescription drugs that can be harmful to unborn babies. You need to discuss any prescription medications with your doctor if you are thinking of becoming pregnant, or as soon as you are pregnant.
Do not take any over the counter medications without first checking with your doctor, pharmacist, or midwife. This includes common drugs such as aspirin or ibuprofen, as well as any complementary or herbal medicines.
It is usually better to avoid taking any non-essential medication, however some medications such as antibiotics are necessary and there are many safe options that can be prescribed. It is important not to stop vital medications without consulting your doctor. For example, asthma medications are safe in pregnancy and it is important that asthma is well controlled when you are pregnant.
ALCOHOL
Alcohol consumed during pregnancy passes directly into the unborn baby’s blood supply. It can have very serious effects on an unborn baby and may even result in a condition called foetal alcohol spectrum disorder (FASD) which has a range of physical, behavioural, and mental effects. The safe level of alcohol during pregnancy is unknown and even a small amount at the wrong time can cause problems. For this reason, women are advised not to drink any alcohol during pregnancy or when they are planning pregnancy.
ILLICIT DRUGS
There are many illicit drugs that can seriously affect your baby’s health if used during pregnancy. These include marijuana, MDMA, cocaine, amphetamines, LSD, and heroin. It is best to avoid all drugs during pregnancy, however, if you are using any drugs be sure to talk to your GP or midwife so they can help you and your baby to stay as healthy and as safe as possible.
SMOKING
It is now well known that smoking causes serious harm to both you and your developing baby. This includes passive smoking, where someone is exposed to another person’s smoking. Smoking in pregnancy can cause complications and is linked with a baby having a low birthweight, being small for age, pre-term birth, some birth abnormalities, and even an increased risk of miscarriage, stillbirth, and SIDS.
The sooner that you stop smoking in pregnancy the better for you and your baby.
TALK TO YOUR GP ABOUT GETTING HELP TO STOP OR REDUCE SMOKING OR CALL THE QUITLINE ON 137 848.
MENTAL HEALTH
Pregnancy and the experience of pregnancy is individual for every woman. Some women find that their mental health remains unchanged or that they may even feel calmer than usual during pregnancy. However some women do experience increased anxiety and/or depression during pregnancy, or in the post-natal period. If you have had mental health concerns before pregnancy then your risk of developing a problem during pregnancy is slightly increased.
If you have concerns about this or feel that you are experiencing some changes to your mood or to your level of anxiety, it is very important to discuss this early with your GP and/or midwife.
If you have a serious mental health issue such as bipolar disorder, borderline personality disorder, schizophrenia or major depressive disorder it is very important that you have the appropriate care and support during your pregnancy. Talk to your GP, midwife and/or mental health professional about your pregnancy and the support services that are available for you.
FOR MORE INFORMATION ABOUT MENTAL HEALTH IN PREGNANCY SEE THE FOLLOWING WEBSITES: BEYOND BLUE AND PANDSI
If you are a client of Mental Health ACT there is a special coordination service called the IMPACT Program that can assist you with managing your care in pregnancy.
THE IMPACT PROGRAM CAN BE ACCESSED TOLL-FREE BY PHONE ON 1800 211 274 FROM 9AM TO 4:30PM WEEKDAYS.
ENVIRONMENTAL TOXINS
There are some common substances that are known to be potentially toxic during pregnancy and are best avoided completely, these are: dry cleaning products, oven cleaners, paint thinners or paint strippers, insecticides, herbicides, and any products or materials which may contain lead or mercury. If you are uncertain about a substance then it is best to avoid it.
MORNING SICKNESS
Morning sickness during pregnancy is common. Symptoms include loss of appetite, aversions to certain foods and smells, nausea, and vomiting. Despite its name it can occur any time of the day or night. There are things you can do to lessen the effects of morning sickness, such as eating very small frequent meals and always avoiding an empty stomach, eating a few dry crackers before getting out of bed in the morning can help, and avoiding any rich, fatty or spicy foods. Occasionally morning sickness can become severe, and in some cases may require hospitalisation. If you experience persistent vomiting see your GP; there are medications that are considered safe to use in pregnancy that can be very helpful in reducing morning sickness.
SEX IN PREGNANCY
Sexual activity in pregnancy is considered quite safe if there are no complications with the pregnancy. Libido in pregnancy is quite individual; some women’s interest in sex decreases but for others it may be unchanged or even increase. It is common for interest in sex to decline as the pregnancy progresses.
PREGNANCY AND BIRTH CARE
PREGNANCY CARE
Care during pregnancy is called antenatal care. Regular antenatal care is very important for the health of you and your baby. This care can be provided by a midwife, a GP, an obstetrician, or a combination of these. The recommended number of visits for antenatal care during pregnancy is 8 to 10.
The first antenatal visit is usually advised before 10 weeks gestation. Your first antenatal visit should include a family history, a medical assessment, a discussion about your model of pregnancy and birth care, test discussions, and planning for ongoing antenatal visits.
TESTS IN EARLY PREGNANCY
There are some important routine blood tests, as well as ultrasound scans that are advised during early pregnancy as part of the health care for you and your baby. You will need to discuss these with your GP.
BIRTH OPTIONS
It is a good idea to start thinking about where you want to have your baby and the kind of care you want to receive during pregnancy and birth as soon as possible. There are a number of choices available. Models of care include a choice of midwife-led continuity of care, public antenatal clinics (available through the Centenary Hospital for Women and Children or Calvary Public Hospital) or private obstetricians.
You may need to book in early for some of these choices, particularly the birth centre or your choice of private obstetrician. Discuss these options with your GP, and if you have private health insurance make sure to check your entitlements for pregnancy and delivery cover.
ANTENATAL AND BIRTH EDUCATION CLASSES
Most hospitals offer free antenatal and birth education classes which will provide you with current information and education about the antenatal period, managing birth, and breastfeeding. There are also private classes available.
FOR MORE INFORMATION ON BIRTH OPTIONS, CLASSES & EDUCATION IN CANBERRA VISIT 'HAVING A BABY IN CANBERRA'.
WHAT SHOULD I DO NEXT?
The next step is to make an appointment to see your GP, or find a GP if you don’t have one.
RECOMMENDED WEBSITES
For reliable evidence-based health information on pregnancy, birth and beyond see:
- Health Direct Australia: Pregnancy.
- The Royal Hospital for Women.
- Having a Baby in Canberra.
- Mothersafe phone counselling service, website, and fact sheets. 9382 6539 or 1800 647848
EARLY PREGNANCY HEALTH AND CARE PDF DOWNLOAD
Last updated April 2019. References: Department of Health (2018) Clinical Practice Guidelines: Pregnancy Care. Canberra: Australian Government Department of Health. Food Safety. RANZCOG. The Royal Women’s Hospital.



